How to reverse aortic stenosis?
Treatment for Severe Aortic Stenosis
- Transcatheter Aortic Valve Implantation. During a TAVI procedure, an interventional cardiologist inserts a replacement valve through an artery in the upper leg.
- Surgical Aortic Valve Replacement. After general anesthesia is administered, a cardiothoracic surgeon makes an incision in the chest. ...
- Deciding Between TAVI and SAVR. ...
How to assess aortic stenosis?
- Role of Cardiac Catheterization. ...
- Role of Computed Tomography. ...
- Potential for Inconsistencies in Diagnostics and Guidelines. ...
- Gorlin Equation. ...
- EOA Versus GOA. ...
- Doppler Versus Catheterization. ...
- Effect of Flow Pulsatility. ...
- Low-Flow, Low-Gradient AS With Reduced EF. ...
- Paradoxical Low-Flow, Low-Gradient AS. ...
- Other Sources of Errors/Inconsistencies. ...
What are the end stages of aortic stenosis?
Stages
- None
- Severe calcification or congenital stenosis with severely reduced opening
- Vmax ≥ 4 m/s or mean ΔP ≥ 40 mmHg
- AVA ≤ 1.0 cm²
- LVEF < 50%
What is the prognosis for severe aortic stenosis?
- Shortness of breath
- Chest pain, pressure, or tightness
- Fatigue
- Feeling lightheaded or dizzy
- Difficulty when exercising or completing day-to-day activities
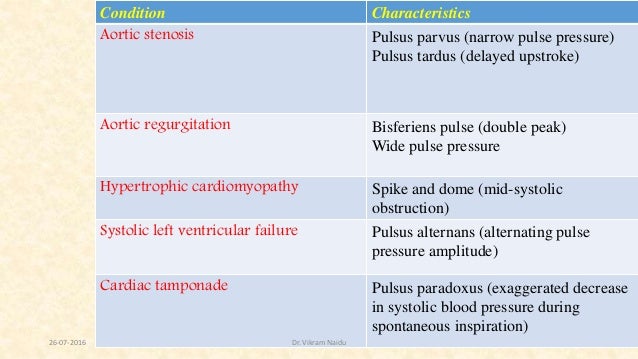
Does aortic stenosis cause wide pulse pressure?
The pulse pressure is the difference between the systolic and diastolic blood pressure. Classically, a wide (high) pulse pressure is a sign of aortic valve regurgitation and a narrow (low) pulse pressure is a sign of aortic stenosis.
Why does narrow pulse pressure occur?
A narrow pulse pressure — sometimes called a low pulse pressure — is where your pulse pressure is one-fourth or less of your systolic pressure (the top number). This happens when your heart isn't pumping enough blood, which is seen in heart failure and certain heart valve diseases.
Why is pulse pressure higher in large arteries than aorta?
Because the aorta is the most compliant portion of the human arterial system, the pulse pressure is the lowest. Compliance progressively decreases until it reaches a minimum in the femoral and saphenous arteries, and then it begins to increase again.
Why does aortic stiffening increase pulse?
Stiffening of the aortic wall and improper matching between aortic diameter and flow are associated with unfavorable alterations in pulsatile hemodynamics, including an increase in forward arterial pressure wave amplitude, which increases pulse pressure.
Why does aortic regurgitation cause wide pulse pressure?
As chronic aortic regurgitation worsens, regurgitant volume increases, as does stroke volume in order to maintain forward cardiac output. This results in increased systolic pressures, reduced diastolic pressures and widened pulse pressure.
What causes a widened pulse pressure?
Pulse pressure naturally increases over time as individuals' age due to arteriosclerosis and diffuse vascular stiffening. However, the differential for widened pulse pressure is broad and includes causes of hyperdynamic circulation and high‐output heart failure, such as aortic regurgitation and hyperthyroidism.
Why is pressure different in the ventricle vs aorta?
Because the aorta is compliant, as blood is ejected into the aorta, the walls of the aorta passively expand to accommodate the increase in blood volume. As the aorta expands, the increase in pressure is determined by the compliance of the aorta at that particular range of volumes.
Why does pressure fluctuate in aorta?
Normal Cardiac Physiology and Ventricular Function A sudden change in aortic pressure is met by a rapid adjustment of coronary vascular resistance so that blood flow remains constant. This autoregulatory phenomenon protects the myocardium from inadequate blood flow owing to a decline in coronary perfusion pressure.
How does a damaged aortic valve affect pulse pressure?
In aortic stenosis, there is a narrowing of the aortic valve, which interferes with the ejection of blood from the left ventricle into the aorta, which results in a decrease in stroke volume and a subsequent decrease in pulse pressure.
How does arterial stiffening affect blood pressure?
Stiff arteries result in higher systolic pressure (because of reduced capacitance). Stiff arteries result in lower diastolic pressure (because there is less elastic recoil to support the diastolic pressure).
How does aorta maintain pressure?
Afterload control Aortic pressure (AoP) is normally maintained by the baroreflex, which adjusts vascular resistance, venous tone, HR, and contractility [30]. However, this mechanism may be diminished in heart failure, partly due to reduced ventricular contractility.
Can arterial blood pressure be normal after aortic valve replacement?
In hypertensive patients with AS, arterial blood pressure may frequently revert to normal values after aor tic valve replacement.4If this would not be the case, antihypertensive medication should be initiated soon thereafter, because a raised blood pressure blunts the favourable regression of left ventricular hypertrophy obtained after valve replacement.
Is hypertension a risk factor for cardiovascular disease?
Hypertension is a well established risk factor for cardiovascular events in the general population. In the absence of large scale cohort studies, the potential impact of coexistent hypertension on the outcome of AS patients is unknown. However, indirect evidence supports the proposal that hypertension may modify the symptomatic status (and hence the need for valve replacement) of AS patients. In an ambispective longitudinal study involving more than 300 patients, we have shown that left ventricular percentage stroke work loss is more useful than the pressure gradient and valve area to determine the outcome of unselected patients with AS.16According to its definition formula, stroke work loss can be interpreted as a blood pressure normalisation of the pressure gradient. Thus, among patients with similar values of valve area and pressure gradient, those with lower blood pressure will develop AS related events sooner during follow up. Irrespective of valve area, higher values of systemic blood pressure seem to account for a less critical disease in terms of outcome.
Does arterial compliance affect Gorlin derived area?
Arterial compliance and vascular resistance may modify Gorlin derived area values by an additional mechanism. Because the transvalvar pressure gradient is inverted during late ejection, we have shown that accounting only for valvar haemodynamics while the pressure gradient is positive may be misleading.15Predictor analysis identified that a low arterial compliance and an increased systemic vascular resistance are direct contributors of a prolonged reverse gradient. Importantly, this source of error can be avoided using the incisura of the aortic pressure tracing to determine the end of the ejection period, instead of using the second left ventricular–aortic pressure crossover.15
Can hypertension cause a carotid pulse?
Therefore, coexisting hypertension may result in a carotid pulse with a rapid upstroke and a normal amplitude, as well as in a diminished murmur or a near normal second cardiac sound. Because of these limitations, an echocardiographic examination should never be obviated if a systolic murmur is found, or if AS is suspected in a hypertensive subject.6
Is low blood pressure a sign of aortic valve stenosis?
Low values of systolic and pulse blood pressure have been classically considered hallmark signs of aortic valve stenosis (AS). However, hypertension has been shown to be independently associated with degenerative calcific aortic valve sclerosis and stenosis in elderly population based studies.1,2Furthermore, in a recent series hypertension was found in one third of patients suffering symptomatic severe AS.3In the absence of specific cohort studies, the nature of the association between AS and high blood pressure is not clear. Involved mechanisms may include a common aetiological pathway, a random coincidence of two highly prevalent diseases, or a true causal relation. Regarding the latter, essential hypertension may constitute a “classical” risk factor for developing AS,1,2but also it seems that AS may cause systolic hypertension.4
Can hypertension affect aortic stenosis?
Hypertension not only can modify the exploratory findings of aortic stenosis, but may also interfere with the assessment of severity, and even have an impact on patient outcome
Is hypertension a problem with AS?
In conclusion, systemic hypertension is nowadays a frequent finding in patients with AS. A raised blood pressure may not only mask the exploratory findings of AS, but can also modify the haemodynamic indices used to assess the severity of the disease. These facts need to be considered for an adequate management of patients with AS.
What happens if your aortic valve is stenosis?
Over time, your aortic valve opening may end up going from the size of a nickel to about the size of the head of a golf tee. This continues to cause more wear and tear on your heart. If your aortic stenosis is severe, you may have the same symptoms as some people with moderate cases -- such as chest pain, tightness, ...
What is aortic stenosis?
In this Article. Aortic stenosis is a type of heart valve disease. Your doctor may classify it as mild, moderate, or severe. Which stage you have depends on how damaged your aortic valve is and the amount of blood that’s still able to pass through it.
How do you know if you have a small aortic valve?
If your condition is moderate, you may notice: Feeling out of breath, especially when you’re active. Chest pain. Tightness or pressure in your chest.
How long does it take for the aortic valve to shrink?
As your aortic valve’s opening slowly starts to shrink with this condition, your heart muscle picks up the slack. It can take many years for this extra work to cause severe damage to your heart muscle. The most common early warning signs are: Needing to make more effort than usual during a physical activity.
What is asymptomatic aortic stenosis?
Because signs of this condition vary so widely, your doctor will want to do tests to see how well your heart is working. Your treatment will be based on your symptoms as well as what these tests show. In severe cases, procedure may be possibly needed to repair or replace your aortic ...
Why does my chest hurt after a lot of activity?
Needing to make more effort than usual during a physical activity. Feeling tired all the time. A child or infant with the condition could also have chest pain after a lot of activity. Because these symptoms are so subtle, most people find out about mild cases during a checkup.
How to tell if you have a heart condition?
If your condition is moderate, you may notice: 1 Feeling out of breath, especially when you’re active 2 Chest pain 3 Tightness or pressure in your chest 4 Heart palpitations (rapid heartbeats) 5 Feeling that your normal exercise has become harder
Study Questions
Is there a link between blood pressure (BP) and outcomes in patients with asymptomatic mild and moderate aortic stenosis (AS)?
Methods
This was a post hoc analysis of data from the SEAS (Simvastatin Ezetimibe in Aortic Stenosis Study) trial, which enrolled patients with asymptomatic mild to moderate AS. Patients with diabetes, congestive heart failure (CHF), or atherosclerosis were not included in the trial.
Results
Over a median follow-up of 4.3 years, 188 subjects died and 504 underwent AVR. There were 95 cardiovascular deaths, 66 strokes, 38 MIs, and 80 episodes of CHF. For the entire population, the lowest event rates were associated with systolic BP 120–139 mm Hg, diastolic BP 70–79 mm Hg, and pulse pressure 60–69 mm Hg.
Conclusions
In patients with asymptomatic mild and moderate AS, optimal BP appears to be 130–139 mm Hg systolic and 70–90 mm Hg diastolic.
Perspective
It is generally presumed that the added pressure burden of hypertension will result in a greater tendency for adverse ventricular remodeling, systolic and diastolic dysfunction, and worsening symptoms in patients with AS. Limited data are available, however, to identify ideal BP targets in patients with AS.