What is a 278 document under HIPAA?
This is an important issue of patient privacy, as 278 documents typically contain healthcare related data, such as patient, diagnosis or treatment information. As of March 31, 2012, healthcare providers must be compliant with version 5010 of the HIPAA EDI standards.
What is a 278 transaction in healthcare?
Unlike other healthcare transactions that may be used in relation to multiple plan subscribers or patients, a single 278 is commonly used for one patient and one patient event. The ANSI X12 EDI standards include three versions of the 278 transaction set.
What is the response to the 278-13 transaction?
From BSC: In response to the 278-13 transactions, the value sent to BSC with ISA record accompanying the 278-13 will be returned on the 278-11 response. 5. Segment Terminator: Byte 106 within the ISA record.
What is a 278 a form?
A 278 may relate to services to be administered by the healthcare service provider, or for referring an individual to another provider. The transaction may also be used by the payer to respond to this request for an authorization.
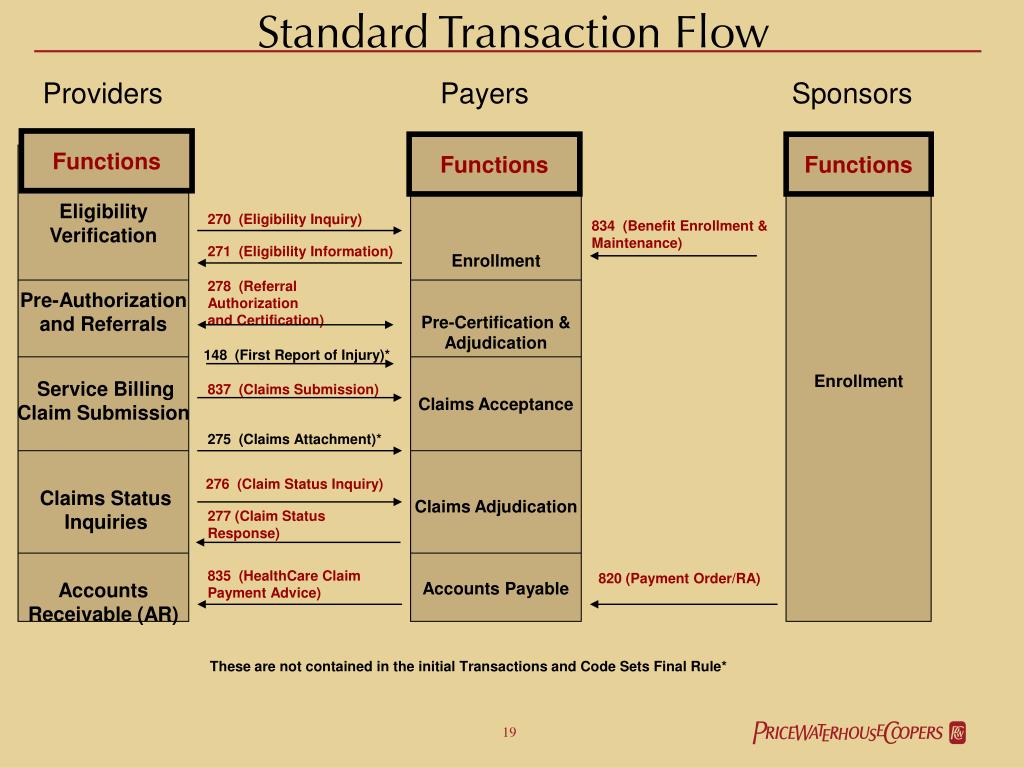
What are the HIPAA X12 transactions?
The key X12 EDI transaction sets specified by HIPAA include: EDI 277-A1 Healthcare Claim Status Notification. EDI 277-A3 Healthcare Claim Status Response. EDI 278-A1 Healthcare Services Review – Request for Review. EDI 278-A3 Healthcare Services Review – Response to Request for Review.
What is a 277 EDI file?
The EDI 277 Health Care Claim Status Response transaction set is used by healthcare payers (insurance companies, Medicare, etc.) to report on the status of claims (837 transactions) previously submitted by providers.
What is a 271 response?
The Eligibility and Benefit Response (271) transaction is used to respond to a request inquiry about the health care eligibility and benefits associated with a subscriber or dependent.
What is ASC X12 5010?
ASC X12 Version 5010 is the adopted standard format for transactions, except those with retail pharmacies. HIPAA standard is used by physicians, clearinghouses, hospitals, pharmacies, payers, and dentists. Some of the most popular messages are 837P, 270, 271, 278, 276, 834, etc.
What is a 270 transaction?
The 270 Transaction Set is used to transmit Health Care Eligibility Benefit Inquiries from health care providers, insurers, clearinghouses and other health care adjudication processors. The 270 Transaction Set can be used to make an inquiry about the Medicare eligibility of an individual.
What is a 276 277 transaction?
The 276 and 277 Transactions are used in tandem: the 276 Transaction is used to inquire about the current status of a specified claim or claims, and the 277 Transaction in response to that inquiry.
What is a 276 transaction?
The EDI 276 transaction set is a Health Care Claim Status Inquiry. It is used by healthcare providers to verify the status of a claim submitted previously to a payer, such as an insurance company, HMO, government agency like Medicare or Medicaid, etc.
What is a 275 transaction?
Electronic Attachments (275 transactions) are supplemental documents providing additional patient medical information to the payer that cannot be accommodated within the ANSI ASC X12, 837 claim format.
What is a 270 271 transaction?
The 270 transaction is the EDI function that requests eligibility and benefit information from the Insurance Company of the patient. It is set to receive care from a Provider of Service. The 271 transaction is the EDI function that responds eligibility and benefit information of the patient.
What is ASC X12 278?
This X12 Transaction Set contains the format and establishes the data contents of the Health Care Services Review Information Transaction Set (278) for use within the context of an Electronic Data Interchange (EDI) environment.
What is the difference between ANSI 4010 and 5010?
The 5010 standards will replace the existing 4010/4010A1 version of HIPAA transactions, which go back nearly a decade—an eternity in the IT world—and address many of the shortcomings in the current version, including the fact that 4010 does not support ICD-10 coding.
What is the 837 file format?
What is an 837 File? An 837 file is an electronic file that contains patient claim information. This file is submitted to an insurance company or to a clearinghouse instead of printing and mailing a paper claim. The data in an 837 file is called a Transaction Set.
What is EDI 278 A3?
Note that a single 278 is commonly used for one patient and one patient event. The EDI 278 A3 transaction set can be used to respond to requests for healthcare service information , such as subscriber, patient, demographic, diagnosis or treatment data.
What is a 278?
A single 278 is commonly used for one patient and one patient event. The Healthcare Services Response document was chosen by HIPAA as the standard format for responses to EDI transmission of authorizations and referrals. This is an important issue of patient privacy, as 278 documents typically contain healthcare related data, such as patient, ...
How many documents are there in the patient privacy report?
This is an important issue of patient privacy, as 278 documents typically contain healthcare related data, such as patient, diagnosis or treatment information.
What is a TA1 response transaction?
If errors are found, a TA1 response transaction will be sent to notify the trading partner that the file could not be processed. No TA1 response transaction will be sent for error-free files.
What is BSC EDI testing?
The purpose of BSC EDI testing phase is to provide you with a mechanism to produce the same reports and acknowledgments that are produced once you are in production. This allows you to test your ability to produce correct data content and to receive and process the acknowledgments and files we produce for you. By testing with BSC EDI, you will be allowed to send transactions. Transactions go from you to BSC Non-Production Environment, as would be the case in a Production Environment. A general breakdown of the process goes like this:
What is the BSC 278?
This specifies the data content for the 278 transaction data that you will be getting from the Blue Shield of California (BSC) Health Plan. BSC has not made any changes or customizations to this format. You may purchase a copy of the 278 implementation guide from the Washington Publishing Company at http://www.wpc-edi.com.
What is companion guide to ASC X12N?
This Companion Guide to the v5010 ASC X12N 278-13 and 278-11 Implementation Guides and associated errata adopted under HIPAA, clarifies and specifies the data content when exchanging eligibility data electronically with Blue Shield of California (BSC) Health Plan. Transmissions based on this companion guide, used in tandem with the v5010 ASC X12N Implementation Guides, are compliant with both ASC X12 syntax and those guides. This Companion Guide is intended to convey information that is within the framework of the ASC X12N Implementation Guides adopted for use under HIPAA. The Companion Guide is not intended to convey information that in any way exceeds the requirements or usages of data expressed in the Implementation Guides.
Can BSC edit trading partner authorization data?
Trading Partners may contact BSC for assistance in researching problems with their transactions. However, BSC will not edit Trading Partner authorization data and/or resubmit transactions for processing on behalf of a Trading Partner. The transaction must be corrected and re-submitted by the Trading Partner.
What is the ASC X12 005010X217?
The ASC X12 005010X217 is the established standard for Request for Review and Response (278).
Does Florida Blue require testing?
Florida Blue recommends that Trading Partners contact Florida Blue to obtain a testing schedule and or notify Florida Blue of potential testing opportunities prior to implementing any foreseen transaction impacts to the business flow of both Florida Blue and /or the Trading Partner.
Payment and remittance advice
This refers to the process where a health plan makes a payment to a financial institution for a healthcare provider.
The Latest on HIPAA Standard Transactions
The Standards for Electronic Transactions and Code Sets were published in 2000. They were subsequently modified in 2010 to include newer standards for several transactions, claims and encounter information, payment and remittance advice, and claims status.
Schedule a Demo for Our HIPAA Compliance Software
ZenGRC is a governance, risk management, and compliance solution that can work to support your HIPAA compliance program.
What are the HIPAA standards?
Under HIPAA, HHS adopted certain standard transactions for the electronic exchange of health care data. These transactions include: 1 Payment and remittance advice 2 Claims status 3 Eligibility 4 Coordination of benefits 5 Claims and encounter information 6 Enrollment and disenrollment 7 Referrals and authorizations 8 Premium payment
Why is HIPAA referred to as administrative simplification?
Together, the provisions are referred to as Administrative Simplification, because their purpose is to simplify the business of health care.
What is a unique identifier?
A standard unique identifier for health plans. Standards for electronic funds transfer and electronic health care claims attachments. These provisions also created a new requirement for health plans to certify their compliance with the adopted standards and operating rules.
What is a 999 TA1?
The TA1 Interchange Acknowledgement and the 999 Functional Group Acknowledgement are used to acknowledge receipt of the 278 Review transaction. The TA1 Acknowledgement responds at the Interchange level of the transmission. The 999 Acknowledgement responds at the Functional Group level of the transmission. The Introduction to the Companion Guide, available online at www.bcbsnc.com/providers/edi/hipaainfo.cfm contains more information on the use of the TA1 and 999 Transactions.
Can BCBSNC process 278-13?
If a 278-13 Review is received, BCBSNC can process the request and provide an automated response on the 278-11; however, the following optional values need to be included in the review in order to receive an automated response:
Does BCBSNC return TA1?
For Technical Report 3 (TR3) violations, BCBSNC returns the TA1 or 999 Acknowledgement Transactions ONLY. Trading partners who are unable to accept a 999 or TA1 transaction are not provided with alternative TR3 error reporting mechanisms.
Who is Dr. Marcus Helby?
Dr. Marcus Helby, a cardiologist, has requested a review for a surgical procedure for Barney Rubble. Reviews for subsequent procedures, to be performed during the same hospitalization, are filed in a separate 278 Review.