What Is Total Opacification of the Maxillary Sinus?
- Causes. There are several possible causes for a CT scan to reveal the maxillary sinus as opaque 1. ...
- Polyps. Polyps can form in the sinus cavities, which can cause poor drainage. ...
- Tumors. Since tumors in the maxillary sinus are often large and appear opaque, they can cause total opacification of the sinus 1.
- Inflammation. ...
- Mucous. ...
What is the treatment for polyP in maxillary sinus?
Treatment
- Medications. Nasal polyp treatment usually starts with drugs, which can make even large polyps shrink or disappear.
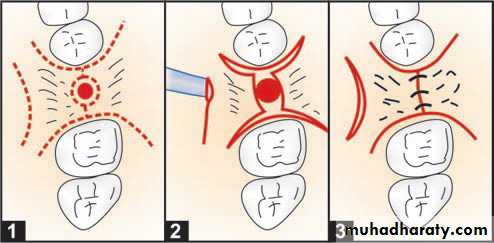
- Surgery. The upper left illustration shows the frontal (A) and maxillary (B) sinuses, as well as the ostiomeatal complex (C).
- Potential future treatments. ...
What does near complete opacification of sphenoid sinus mean?
Sphenoid sinusitis is an inflammation-related condition that can create uncomfortable symptoms and headache pain. Here, we explore what causes sphenoid sinusitis and how to deal with it.
What are the surgical options for Chronic Maxillary Sinusitis?
- Facial pain, pressure or fullness
- Headaches
- Difficulty breathing through nose
- Decreased sense of smell
- Drainage of cloudy or colored mucus
What causes solitary polyp in the maxillary sinus?
What causes solitary polyp in the maxillary sinus?
- Drink plenty of warm water. Warm water helps in hydrating the nasal tissues and thus prevents any cracking of the skin inside the nose.
- Use saline nasal spray. It functions in the similar as above.
- Do steam inhalation 2-3 times a day for at least 3 min. ...
- Avoid forceful blowing of the nose or nose picking.
See more
What causes complete opacification of maxillary sinus?
Mucoceles are most often caused by sinus ostial obstruction that leads to complete opacification of the sinus because of an accumulation of secretions. In many instances, the entire sinus may be expanded on radiologic imaging.
What does complete opacification of maxillary sinus mean?
2) while partial opacification was defined as at least one-third of the maxillary sinus being opacified without clear distinct boundaries (Fig. 3). Complete opacification was a completely opacified maxilla in all axial and coronal slices (Fig.
Is sinus opacification serious?
Isolated sphenoid sinus opacifications (ISSOs) are clinically important because they can lead to serious complications. However, some patients with ISSOs are asymptomatic, and not all patients are properly referred to the otolaryngology department.
What does completely Opacified mean?
Medical Definition of opacify transitive verb. : to cause (as the cornea or internal organs) to become opaque or radiopaque. intransitive verb. : to become opaque or radiopaque.
What causes mucosal thickening in maxillary sinus?
Mucosal thickening is an inflammatory reaction with hyperplasia of the mucous lining of the maxillary sinus. This condition may result from harmful actions caused by trauma, infections, chemical agents, foreign body reaction, neoplasm, or airway conditions such as allergies, rhinitis, or asthma.
What causes calcification in sinus cavity?
As previously reported (2–6), intrasinus calcification is commonly found in fungal sinusitis, usually aspergillosis. Intrasinus calcification can also occur in nonfungal inflammatory diseases of the paranasal sinus, such as mucocele or bacterial sinusitis.
What does Opacified mean in sinuses?
The polyp opacifies and slightly enlarges the sinus cavity with no bone destruction. The enlarged antral polyp protrudes through the maxillary infundibulum or accessory ostium into the middle meatus and then the posterior choana, with possible extension into the posterior nasopharynx.
Is maxillary sinusitis serious?
This condition is rarely life-threatening, but it can be dangerous at times. Infections can spread beyond the sinuses into your bones, brain or spine.
How do you treat maxillary sinusitis?
Rather, treatment is based on topical nasal decongestants and saline irrigation of the nasal cavity. Topical decongestants such as ephedrine or xylometazoline constrict the nasal lining, widening the paranasal sinus ostia, facilitating drainage by ciliary activity.
What causes opacification?
The opacification is caused by fluid or solid material within the airways that causes a difference in the relative attenuation of the lung: transudate, e.g. pulmonary edema secondary to heart failure. pus, e.g. bacterial pneumonia. blood, e.g. pulmonary hemorrhage.
What does opacification mean on CT scan?
Pulmonary opacification represents the result of a decrease in the ratio of gas to soft tissue (blood, lung parenchyma and stroma) in the lung. When reviewing an area of increased attenuation (opacification) on a chest radiograph or CT it is vital to determine where the opacification is.
What is maxillary sinus disease?
Maxillary Sinusitis is the inflammation of the paranasal sinuses caused by a virus, bacteria, or fungus. The infection can also result after an allergic reaction – when the immune system attacks the healthy body cells. This infection may be associated with both bacterial and fungal infections.
Why is my sinus opacified?
Total opacification of the maxillary sinus is a symptom of acute sinusitis which, according to MedScape, can be caused by an infection, structural variations in the nasal cavity, allergic responses or nasociliary malfunction. Sinonasal polyps are another condition that show up as opacified areas on a scan.
What is the opacified area on a sinus scan?
Sinonasal polyps are another condition that show up as opacified areas on a scan. The maxillary sinuses are open cavities inside the maxilla, which is the upper jaw bone that extends upward on either side of the nose to the eye sockets.
What is the maxillary sinus?
The maxillary sinus is the paranasal sinus that impacts most on the work of the dentist as they will often be required to make a diagnosis in relation to orofacial pain that may be sinogenic in origin. Maxillary sinus disease is often coincidentally observed on radiographs, and dentists often have to make a diagnosis and plan treatment based on the interpretation of the image. This paper aims to guide the dental professional through some of the disease processes involving the paranasal sinuses and in particular the maxillary sinus. The outcome is to encourage comprehensive history taking and examination of the patient to facilitate an accurate diagnosis that will enable successful treatment.
What is the direction of mucociliary activity in the maxillary sinus?
The direction of mucociliary activity in the maxillary sinus is in blue. Ethmoid polyps are in red, with antrochoanal polyps in green. Full size image. The ostium of the maxillary sinus is high up on the medial wall and on average is 2.4 mm in diameter.
What is the most common disease in the paranasal sinuses?
Inflammatory sinus disease is the most common disease process involving the paranasal sinuses. 3 When the maxillary sinus is involved, it is the disease entity where a dentist will most often be asked to make a differential diagnosis.
What is the most common fungal disease in the maxillary sinus?
Most fungal disease of the maxillary sinus involves the organism Aspergillus which lives within moulds and spores and is regularly inhaled into the respiratory system. When infection occurs with Aspergillus in relation to dental foreign materials, the infection is normally contained within the confines of the maxillary sinus. 20 Foci of infection may lead to dystrophic calcification and the formation of rhinoliths, which may be seen on dental radiographs. ( Fig. 12) Large rhinoliths are known as fungal balls. Treatment is normally surgical with removal of any predisposing cause, and this is also increasingly being provided endoscopically with the aim of restoring normal mucociliary function.
What is the process of growth of the sinuses?
Growth of the sinus continues through life by a process called pneumonisation, such that the roots of maxillary teeth often project into the air space, and following loss of teeth, the sinus floor may be at a level below the nasal floor. The right and left sinuses are often of different dimensions.
What is dome shaped radiopacity?
The non-corticated, dome-shaped radiopacity within the maxillary sinus is a retention cyst and not related to the dental disease. The bone density of the hard palate is superimposed on the maxillary sinus
What is the treatment for acute sinusitis?
Treatment of acute sinusitis is based on relief of symptoms and does not involve antibiotics unless the patient is pyrexial or there is evidence of spread of infection beyond the confines of the sinus. 8 Rather, treatment is based on topical nasal decongestants and saline irrigation of the nasal cavity.
Image Gallery
Sinonasal inflammatory disease with sinus ostial obstruction is a very common cause of an opacified paranasal sinus. However, there is a differential for an opacified paranasal sinus (Table 1).
Inflammation
Sinonasal inflammatory disease with sinus ostial obstruction is a very common cause of an opacified paranasal sinus. An air-fluid level suggests acute sinusitis; in chronic sinus disease, one may see mucosal thickening and sclerosis of the bony sinus walls. 1 The sinus is normal in size.
Silent sinus syndrome (SSS)
Both silent sinus syndrome (SSS) and the mucocele, which is discussed in the next section, are characterized by abnormal sinus size, with reduced sinus volume in SSS and sinus expansion in mucocele.
Mucocele
By definition a completely opacified, nonenhancing and mucus-filled expanded sinus, a mucocele is the most common expansile mass of a paranasal sinus (Figure 3). Most often secondary to an obstruction of the sinus ostium, mucoceles may also result from surgery, osteoma or prior trauma; this is especially true of frontal sinus mucoceles.
Mycetoma
Mycetoma, also known as a “fungus ball,” is a manifestation of fungal sinus disease. Fungal sinusitis is broadly categorized as invasive or noninvasive, with five major subtypes. The noninvasive subtypes typically occur in immunocompetent individuals and include mycetoma and allergic fungal sinusitis.
Dentigerous cyst
Both dentigerous cysts and ameloblastomas, which are discussed in greater detail in the next section, originate in the bony maxilla and may then secondarily involve the adjacent maxillary sinus.
Ameloblastoma
Ameloblastoma is the most common odontogenic tumor. Defined as a benign epithelial neoplasm, the tumor is locally aggressive and invasive. Incomplete resection may result in local persistence or recurrence or, rarely, distant typically pulmonary metastases.
How many patients underwent sinus surgery in 1995?
From August, 1, 1995, to July 31, 1997, 510 patients underwent sinonasal surgery for the treatment of chronic maxillary sinusitis. Four hundred fifty-one patients had functional endoscopic sinus surgery and 59 patients had Caldwell-Luc operations. Noncontrast CT examinations were performed for presurgical assessment in all patients. Two radiologists retrospectively assessed the CT scans to determine whether calcification was present in the maxillary sinuses that had been treated surgically owing to chronic inflammation. Thirty-six of 510 patients had intrasinus calcification on CT scans. The organisms causing sinusitis were pathologically proved by endoscopic sinus surgery in 34 patients and by Caldwell-Luc operation in two patients. The patients included 14 men and 22 women, ranging in age from 18 to 77 years.
Why is it important to differentiate fungal sinusitis from nonfungal sinusitis?
BACKGROUND AND PURPOSE: It is important to differentiate fungal from nonfungal sinusitis in order to determine the optimal treatment for chronic sinusitis. The purpose of this study was to describe the CT findings of calcifications in chronic fungal and nonfungal maxillary sinusitis.
What is intrasinus calcification?
Intrasinus calcification is found in a variety of diseases, including inflammatory conditions and benign or malignant tumors (1). As previously reported (2–6), intrasinus calcification is commonly found in fungal sinusitis, usually aspergillosis. Intrasinus calcification can also occur in nonfungal inflammatory diseases of the paranasal sinus, ...
What stain was used to confirm the presence of fungal hyphae?
Hematoxylin-eosin was used as a routine staining method, and Gomori's methenamine silver stain was used to confirm the presence of fungal hyphae.
Can sinusitis cause intrasinus calcification?
Intrasinus calcification can also occur in nonfungal inflammatory diseases of the paranasal sinus, such as mucocele or bacterial sinusitis. However, intrasinus calcification is uncommon in nonfungal inflammatory sinonasal disease and there is little literature concerning intrasinus calcification in nonfungal sinusitis (1, 6). ...
Is calcification found in sinusitis?
Calcification with a nodular or linear shape was found with both fungal and nonfungal sinusitis; however, fine punctate calcification was found only in fungal sinusitis, while smooth-margined, round, or eggshell type calcification was found exclusively with the nonfungal variety.