Full Answer
Does Anthem Blue Cross cover rehab?
If a prospective rehab patient carries Anthem Blue Cross insurance, the cost of their treatment may be covered. But it depends on their specific insurance policy, and if the rehab or detox center they wish to attend accepts Anthem Blue Cross insurance.
Does anthem cover Accutane?
The Anthem Drug List, also called a formulary, is a list of U.S. Food and Drug Administration (FDA)-approved brand-name and generic drugs that have been ... it does not guarantee coverage. Some drugs, such as those used for cosmetic purposes, may be excluded from ... Accutane (isotretinoin)* Aceon (perindopril)* Aci-Jel Jelly (acetic acid vaginal)*
Does Anthem Blue Cross cover chiropractic?
Or you might have health insurance, but it won’t cover chiropractic treatment or physical therapy type treatments. What does Blue Cross Blue Shield dental cover? It doesn’t cover routine dental exams, cleanings, procedures or dentures. It does cover some dental care related to hospitalizations, surgeries and the treatment of diseases.
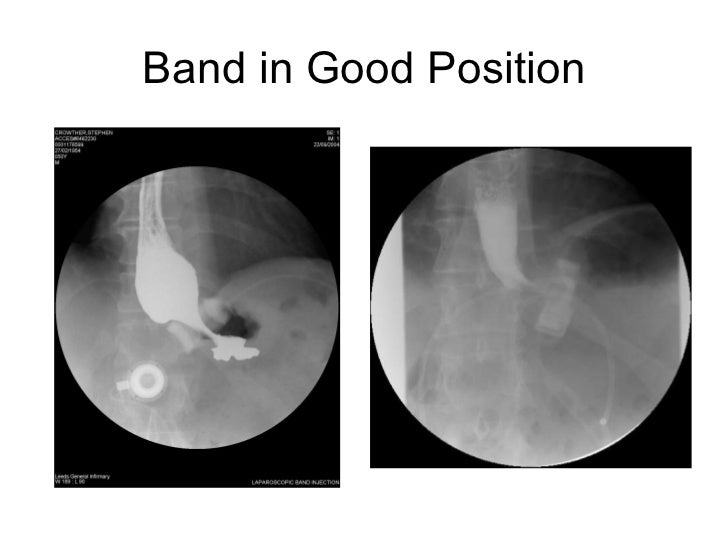
Does Anthem Blue Cross cover lap band surgery?
Yes, Anthem Blue Cross covers lap band surgery provided you fulfill the eligibility criteria for this weight loss procedure. Make sure to carefully go through your insurance policy document to know which expenses related to your lap band surgery are covered. It’s always a wise idea to call your insurer and ask them to verify your actual Anthem Blue Cross lap band surgery coverage for you.
Why is weight loss surgery not covered by insurance?
From the insurance perspective, weight loss surgery has always been considered “medically necessary.” This means that weight loss surgery is not considered cosmetic, but rather is performed to decrease the health risks associated with severe obesity.
How long does it take for insurance to cover gastric sleeve?
It can take two to four weeks for the insurance company to respond with a decision.
What can disqualify you from bariatric surgery?
Exclusions for weight loss surgeryDrug and/or alcohol addiction.Age under 16 or over 75.History of heart disease or severe lung problems. ... Chronic pancreatitis (or have a history of this).Cirrhosis of the liver.Autoimmune disease such as systemic lupus erthyematosus.More items...
Is it hard to get approved for gastric sleeve?
You typically qualify for bariatric surgery if you have a BMI of 35-39, with specific significant health problems like Type 2 diabetes, sleep apnea or high blood pressure. A BMI of 40 or higher also is a qualifying factor.
How to contact the national anthem?
You can contact Anthem’s customer service at 1-866-293-2892. You can also look on their website www.anthem.com for the email address and contact number.
What is covered by revisions?
Revisions may be covered if documentation of a failure or a surgical complication such as obstruction, fistula or disruption of staple or suture line.
Does insurance cover gastric sleeves?
Some large insurance companies have started covering gastric sleeves. However, this procedure is considered experimental and is not covered. The following surgeries are covered:
Does Blue Cross Blue Shield cover obesity?
Obesity Coverage feels very strongly that morbid obesity is a serious illness and that all insurance companies need to cover the life-saving techniques. The majority of the Blue Cross Blue Shield network has some kind of weight loss surgery coverage.
Do you have to use an in-network surgeon for weight loss surgery?
The surgery must take place at a Center of Excellence. However, you do not have to use an in-network surgeon. But, the costs will be higher for you if you use an out of network doctor. They will also need to have privileges to perform the weight loss surgery at the accredited Center of Excellence.
Does BCBS cover lap band fills?
For example, you had an modifiable gastric banding procedure that met every criteria for it. If cash paid for the weight loss procedure, the insurance will not cover continuous lap band fills.
What is the trade name for the anthem BCBS?
Blue Cross of California is the trade name for Anthem BCBS so your criteria for weight loss surgery will be the same as it is here.
What are revisions covered by?
Revisions are covered if there is documentation of a failure secondary to a surgical complication. Complications can include but are not limited to fistula, obstruction or disruption of a suture/staple line.
Is lap banding covered by insurance?
This is true only if you’ve had a previous adjustable gastric banding procedure that met all of the criteria laid out for that procedure. Typically , if you paid cash for the procedure ongoing lap band fills will not be covered by insurance.
Does the national anthem cover weight loss surgery?
Anthem’s full policy on weight loss surgery insurance coverage is no longer available online. The best option is to call them directly and ask if your policy includes coverage for CPT Code 43775. This is the medical billing code for gastric bypass surgery.
Does Blue Cross Blue Shield cover weight loss?
In fact, most of the Blue Cross Blue Shield network has some sort of coverage for weight loss surgery. It is important to know that your employer can typically opt-out of weight loss surgery insurance coverage for their employees’ policies. Opting-out typically saves the company money on their premiums. Contact information for your Anthem BCBS is ...
Does BCBS cover weight loss surgery?
Anthem BCBS may cover weight loss surgery as long as your policy does not specifically exclude coverage. ObesityCoverage strongly feels that morbid obesity is a disease and every insurance company should cover these life saving procedures.
How many strictures are there after bariatric surgery?
The incidence of strictures following bariatric procedures vary based on the initial surgical procedure but is generally reported to be between 1-2% and 16-23.0%. Treatment options include endoscopic balloon dilation, endoscopic dilatation with or without stenting and resection of the stricture to conversion to another procedure, generally RYGB (Brethauer, 2014).
What is operator dependence in bariatric surgery?
Evidence from a number of reports and case series exists for “operator dependence” in determining the risks and benefits of any bariatric procedure. It is important that the surgeon be extensively trained in the respective procedure and that the initial surgeries are supervised by an experienced bariatric surgeon during the early “learning curve.” It is also important that these surgeries be performed in facilities that are appropriately qualified to support peri-operative and post-op services by an appropriately trained, multi-disciplinary team to ensure maximal success.
What are the two types of surgery for obesity?
Surgery for clinically severe obesity (bariatric surgery) falls into two categories: gastric restrictive procedures and malabsorptive procedures.
What BMI should I have for metabolic surgery?
The 2021 American Diabetes Association (ADA) Standards of Medical Care in Diabetes notes that metabolic surgery “should be recommended as an option” in adults with type 2 diabetes with a BMI of 40 kg/m 2 (BMI ≥ 37.5 kg/m 2 in Asian Americans) or a BMI of 35.0-39.9 kg/m 2 (32.5 -37.4 kg/m 2 in Asian Americans) who “do not achieve durable weight loss and improvement in comorbidities (including hyperglycemia) with reasonable nonsurgical methods.” The ADA standards note that metabolic surgery “may be considered as an option” in adults with type 2 diabetes is a BMI of 30.0-34.9 kg/m 2. The document notes:
Is bariatric surgery safe for T2DM?
Bariatric surgery has been investigated as a treatment for type 2 diabetes mellitus (T2DM). To date, studies reporting the results of bariatric surgery on T2DM have primarily included individuals with morbid obesity (that is, with a BMI greater than or equal to 40 or 35-39.9 kg/m 2 with a clinically significant obesity-related comorbidity). There have been very few studies that investigated the safety and efficacy of bariatric surgery, also referred to as metabolic surgery, in individuals with a BMI less than 35 kg/m 2. In 2012, Mingrone published results of a single-center, nonblinded, RCT of 60 subjects between the ages of 30 and 60 years with a BMI of 35 or more and a history of at least 5 years of diabetes. Study participants were randomly assigned to receive conventional medical therapy or bariatric surgery (either GB or BPD). The primary endpoint was the rate of diabetes remission at 2 years (defined as a fasting glucose level of < 100 mg per deciliter [5.6 mmol per liter] and a glycated hemoglobin level of < 6.5% in the absence of pharmacologic therapy). At 2 years, diabetes remission had occurred in no subjects in the medical-therapy group versus 75% in the GB group and 95% in the BPD group (p<0.001 for both comparisons). Age, sex, baseline BMI, duration of diabetes, and weight changes were not significant predictors of diabetes remission at 2 years or of improvement in glycemia at 1 and 3 months. At 2 years, the average baseline HbA1c level (8.65 ± 1.45%) had decreased in all groups, but subjects in the 2 surgical groups had the greatest degree of improvement (average HbA1c levels, 7.69 ± 0.57% in the medical-therapy group, 6.35 ± 1.42% in the GB group, and 4.95 ± 0.49% in the BPD group). The authors concluded that, in severely obese subjects with T2DM, bariatric surgery resulted in better glucose control than did medical therapy and that preoperative BMI and weight loss did not predict the improvement in hyperglycemia seen after surgery (Mingrone, 2012).
Is reoperative bariatric surgery better than primary surgery?
The risks of reoperative bariatric surgery are higher than with primary bariatric surgery and the evidence highlights the need for careful patient selection and surgeon expertise.
Is OAGB a good weight loss procedure?
While OAGB is used in other countries, it is not considered to be a clinically appropriate for the treatment of obesity in the United States at this time. The American Society for Metabolic and Bariatric Surgery (ASMBS) does not recommend OAGB as a primary weight loss procedure.
How long does weight loss surgery cover?
Weight-related revision procedures are usually covered 2 or more years after the primary surgery and are based on the amount of weight lost.
What Procedures Are Covered?
Procedures considered experimental, like the Mini Bypass will not be covered. Band fills are covered if you had a gastric band using your insurance, but not for cash pay. The gastric balloon is not yet covered by insurance and we do not offer it for a number of reasons.
Does A Preapproval Mean Guarantee Coverage?
Preapproval for coverage does not automatically guarantee payment. There are various reasons that the insurance company can deny your claim. Once again, many of these are administrative mistakes that are easily fixed. You have the option to appeal your denial to the insurance company should resubmitting your claim fail once again.
What is the largest health insurance in Georgia?
Anthem Blue Cross Georgia is the largest health insurer in the state with over 1,000,000 policies and over 30% market share. As a result, Blue Cross is often at the forefront of insurance company policy changes as they relate to coverage of bariatric surgery and other procedures.
What are comorbidities in insurance?
Qualifying comorbidities include high blood pressure, high cholesterol, sleep apnea, osteoarthritis, type 2 diabetes and more. History of failed diet and exercise. Your insurance company will expect you to provide proof of failure in diet and exercise programs.
What is pre-op weight loss?
Pre-op weight loss programs. Most policies require participation in a weight loss program before pre approval for weight loss surgery. This program will consist of diet and lifestyle change and may include medication management. Comorbidities.
Does BCBS cover bariatric surgery?
If your BCBS insurance policy covers bariatric surgery, you will be required to meet a certain set of criteria to be eligible for coverage and receive a pre approval for surgery. These criteria can vary dramatically between insurance companies and even between policies, so it is important that you understand your specific policy terms and only to use the below as a guide.
What to do if Blue Cross Blue Shield bariatric surgery is denied?
In a situation where Blue Cross Blue Shield bariatric surgery policy coverage is denied, check for clerical errors and ask for a reason.
What kind of doctor do you need for bariatric surgery?
Psychological evaluation: An independent, licensed psychiatrist or behavioral specialist may have to carry out a professional psychological before your scheduled bariatric surgery to determine your mental and emotional fitness to undergo the procedure.
What BMI do you need to be to get lap band surgery?
Your co-morbidities will be evaluated if your BMI is less than 40 before you get Anthem Blue Cross lap band surgery authorization.
How long do you have to have a morbid obesity diagnosis for Blue Cross Blue Shield?
Obesity diagnosis: To be eligible for coverage under Blue Cross Blue Shield federal weight loss surgery program, you may have to present medical records showing morbid obesity diagnosis for up to three years. Correlating with this, you may submit your PCP’s attestation to this effect.
Does Blue Cross cover gastric sleeve surgery?
Coverage can vary: Each Blue Cross and Blue Shield health plan can vary regarding which gastric sleeve surgery expenses are covered. Talk to your insurance agent to verify the available coverage for you by filling out the free, no-obligation verification form. This will give you clarity on actual amount of coverage.
Is gastric sleeve covered by Blue Cross Blue Shield?
Blue Cross Blue Shield gastric sleeve is a covered procedure under many types of insurance plans for qualified individuals. Gastric sleeve is currently the most popular form of bariatric surgery with an excellent success rate. Therefore, as long as you meet the eligibility conditions, you should be able to obtain approval from your insurance company without much difficulty.
Does Blue Cross cover lap band fills?
Lap band fills cost is included in your Anthem Blue Cross lap band coverage, if your prior lap band surgery met the required conditions.
What is a bariatric evaluation?
An evaluation within the past 12 months, including an assessment by a surgeon qualified to perform bariatric surgery recommending surgical treatment, a separate medical evaluation recommending bariatric surgery, clearance for surgery by a mental health provider and a nutritional evaluation by a physician or registered dietician.
What to do if your insurance doesn't cover surgery?
You will probably need to provide further documentation of your need for the surgery as medically necessary. All health insurance plans should have a clear appeals process. Find out what it is and follow directions.
How long does it take Medicaid to approve weight-loss surgery?
Medicaid also allows weight-loss surgeries if you meet criteria, but recent studies show approval make take longer.
What BMI do I need to be on Medicare?
Similar to other insurers, Medicare will likely require a BMI of at least 35, your weight must also be causing serious health issues and you’ve attempted for years to lose weight through diet and exercise.
What is the BMI for weight loss surgery?
Have a BMI of 40 or higher. Have A BMI of between 35 and 40 and weight-related health problems, such as type 2 diabetes and high blood pressure.
Does Aetna cover bariatric surgery?
Aetna doesn’t offer any individual health plan that covers bariatric surgery. Most Aetna group HMO and POS plans exclude coverage of surgical operations, procedures or treatment of obesity unless approved by Aetna.
How long does it take to appeal a health insurance claim?
You may only have a limited time from the date you were denied or had the procedure to get an appeal underway, possibly only 60 days. Depending on your plan's procedure, you might have to start with a phone complaint and then move to a written appeal.